Nodal T-follicular helper cell lymphoma (nTFHL) is a subset of peripheral T-cell lymphoma (PTCL) characterized by a distinct immunophenotype (such as CD10, BCL6, CXCL13, PD1, and ICOS) and mutations (including TET2, RHOA G17V, and IDH2 R172). However, the impact of molecular classification based on genetic profiling on prognosis in nTFHL remains largely unknown.
Here we performed targeted-capture sequencing (targeted-seq) covering 235 T/NK-cell lymphoma-related genes with a mean depth of 526×. Then, we analyzed 49 genes which were reported as drivers in the previous PTCL studies to reveal the associations between clinical phenotypes and somatic alterations in a cohort of 153 patients whose clinical information was available and who were pathologically diagnosed with nTFHL according to the WHO-HAEM5. When mutation and copy number alteration (CNA) data were combined, we identified recurrent alterations in 40 among 49 driver genes. TET2 was most frequent (68%), followed by RHOA (51%), IDH2 (27%), DNMT3A (20%), PLCG1 (9%), TP53 (7%), KMT2C (6%), VAV1 (6%), CD28 (6%), KMT2D (6%), NOTCH1 (5%), and CDKN2A (5%).
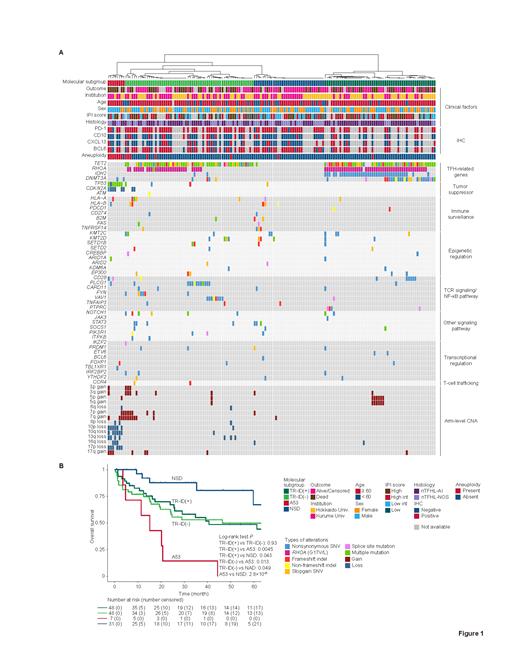
To create a molecular classification based on genetic alterations in nTFHL, we conducted hierarchical clustering using driver alterations and arm-level CNAs. This analysis identified four molecular subgroups named after their characteristic genetic alterations ( Fig. 1A). TR-ID (+) ( n = 52) and TR-ID (-) ( n = 60) were defined by TFH-related mutations ( TET2 and RHOA). Among them, TR-ID (+) harbored IDH2 and/or DNMT3A mutations. A53 ( n = 8) was notable for biallelic inactivation of TP53 and/or CDKN2A and associated with marked aneuploidy. NSD ( n = 33) had no subgroup-defining alterations with the fewest number of mutations. Clinically, TR-ID (+) tumors were mostly nTFHL-angioimmunoblastic-type (AI), which is consistent with the enrichment of IDH2 and/or DNMT3A mutations. On the other hand, TR-ID (-) tumors exhibited a higher proportion of nTFHL-NOS. NSD exhibited lower LDH levels and was significantly associated with younger age and localized stage than other subgroups. A53 showed the worst prognosis with a median overall survival (OS) of 15.1 months (mos) ( Fig. 1B). By contrast, the OS of NSD was significantly superior to the others (median OS not reached). The OS of TR-ID (+) and TR-ID (-) was comparable with a median OS of 40.6 and 46.4 mos, respectively. Notably, A53 remained significant in multivariate analyses adjusted for IPI or PIT score. Thus, genetic profiling enables to classify nTFHL patients into genetically and clinically distinct subgroups, including the unfavorable prognostic subgroup (A53).
Next, to identify potential genes linked to the poor prognosis of the A53 subtype, we examined the prognostic impact of individual alterations. Among the genes examined, TP53 and CDKN2A, hallmarks of A53, were significantly associated with shorter OS in univariate analysis. Consequently, cases with TP53 and/or CDKN2A alterations showed a poor prognosis (median OS 11.4 vs 181.2 mos, P = 8.2×10 -7), thereby reinforcing the negative prognostic impact of A53.
Then, we investigated other prognostic factors within each molecular subgroup. First, in TR-ID (+) and (-) cases, we examined the EBV status, which was known to be associated with worse prognosis in nTFHL-AI. Among them, 22 (16%) cases were EBV-positive. Despite no observed differences in genetic and clinical factors, EBV-positive cases exhibited a worse prognosis (median OS 66.5 vs 14.9 mos, P = 0.0018). Next, we assessed the influence of TCR clonality on prognosis in NSD cases. The clonal T-cell fraction assessed by targeted-seq was highest in A53 (median, 75%) but lowest in NSD (median, 16%). OS of NSD cases was further stratified by T-cell clonality (median OS not reached vs 67.7 mos for low and high clonal T-cell fraction; P = 0.042), while the presence of driver alterations failed to predict the prognosis. These findings suggest that assessment of T-cell clonality helps to identify the favorable prognostic subgroup characterized by low tumor content.
In summary, we defined four molecular subgroups with different clinical features and also clarified subgroup-specific prognostic factors in nTFHL. Particularly, we identified the molecular subgroup with unfavorable prognosis (A53) for which different clinical approach should be warranted. This classification will refine the patient prognostication and stratification in nTFHL.
Disclosures
Hatanaka:SEKISUI: Research Funding; Eli Lilly: Research Funding; NEC: Research Funding. Kogure:Daiichi Sankyo Co., Ltd.: Honoraria; Kyowa Kirin Co., Ltd.: Honoraria; Nippon Shinyaku Co., Ltd.: Honoraria; Takeda Pharmaceutical Co., Ltd.: Honoraria. Koya:TOMY DIGITAL BIOLOGY CO.,LTD.: Honoraria. Teshima:Asahi Kasei Pharma: Membership on an entity's Board of Directors or advisory committees, Research Funding; NIPPON SHINYAKU: Honoraria, Research Funding; Eisai: Research Funding; AbbVie: Honoraria; Priothera SAS: Research Funding; Kyowa Kirin: Honoraria, Research Funding; Astellas: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; SHIONOGI: Research Funding; Otsuka: Research Funding; Bristol-Myers Squibb: Honoraria; ONO: Research Funding; LUCA Science: Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck Sharp & Dohme: Honoraria; Sumitomo Pharma: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Fuji Pharma: Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; Roche Diagnostics: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Meiji Seika Pharma: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; DAIICHI SANKYO: Membership on an entity's Board of Directors or advisory committees; Chugai: Honoraria, Research Funding. Hatanaka:Eli Lilly: Honoraria, Research Funding; Shionogi: Research Funding; NEC: Consultancy, Research Funding; DaiichiSankyo: Honoraria, Research Funding; Sysmex: Research Funding; Astrazeneca: Honoraria; Merck: Honoraria; Novaltis: Honoraria; MSD: Honoraria. Kataoka:Janssen Pharmaceutical: Honoraria; Sumitomo Pharma: Honoraria, Other: Scholarship; AstraZeneca: Honoraria; Chugai Pharmaceutical: Honoraria, Other: Scholarship, Research Funding; Kyowa Kirin: Honoraria, Other: Scholarship; Nippon Shinyaku: Honoraria, Other: Scholarship; Pfizer: Honoraria; Bristol Myers Squibb: Honoraria; SymBio Pharmaceuticals: Honoraria; Takeda Pharmaceutical: Honoraria, Other: Scholarship, Research Funding; Ono Pharmaceutical: Honoraria; Eisai: Honoraria, Other: Scholarship; Novartis: Honoraria; Daiichi Sankyo: Honoraria, Other: Scholarship; Alexion Pharmaceuticals: Honoraria; AbbVie: Honoraria; Meiji Seika Pharma: Honoraria, Research Funding; Sanofi: Honoraria; Sysmex: Honoraria; Mundipharma: Honoraria; Incyte Corporation: Honoraria; Kyorin Pharmaceutical: Honoraria; Asahi Kasei Pharma: Other: Scholarship; Otsuka Pharmaceutical: Other: Scholarship, Research Funding; Shionogi: Other: Scholarship; Teijin Pharma: Other: Scholarship; Japan Blood Products Organization: Other: Scholarship; Mochida Pharmaceutical: Other: Scholarship; JCR Pharmaceuticals: Other: Scholarship; Nippon Kayaku: Other: Scholarship; Chordia Therapeutics: Research Funding. Nakagawa:AbbVie Inc.: Research Funding; Meiji Seika pharma: Honoraria; Astrazeneca: Honoraria; Mundipharma: Honoraria; Takeda Pharmaceutical Company Limited: Honoraria, Research Funding.